What is Plantar Fasciitis?
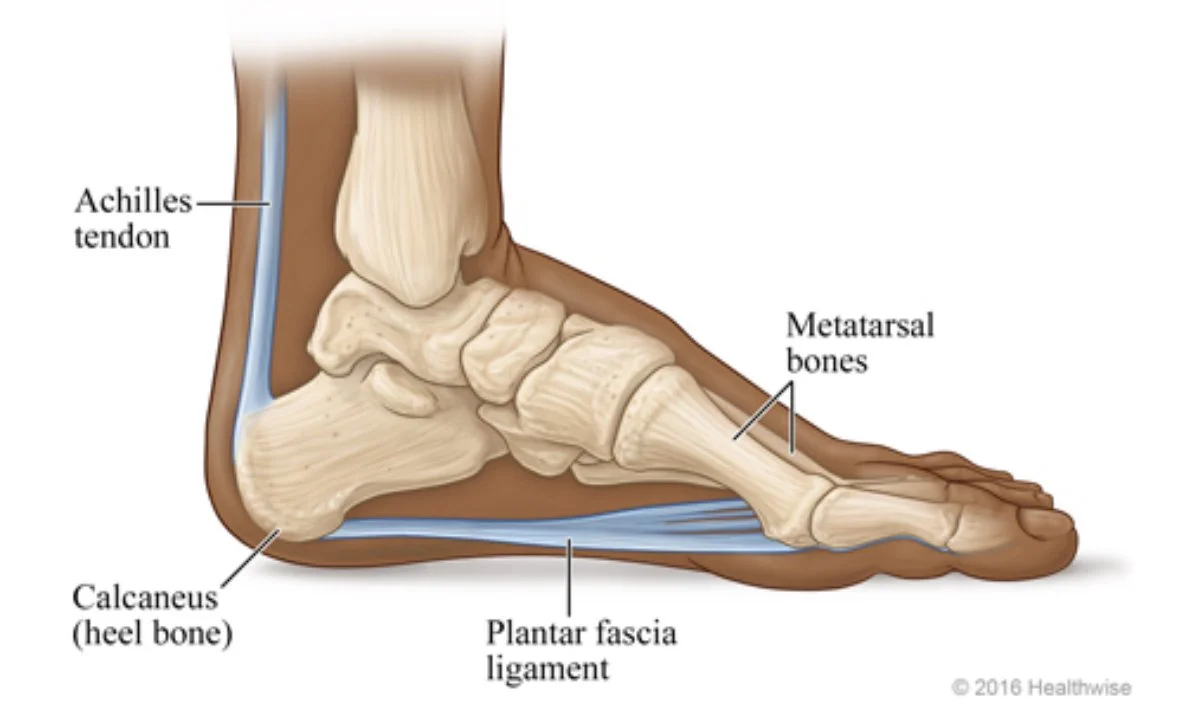
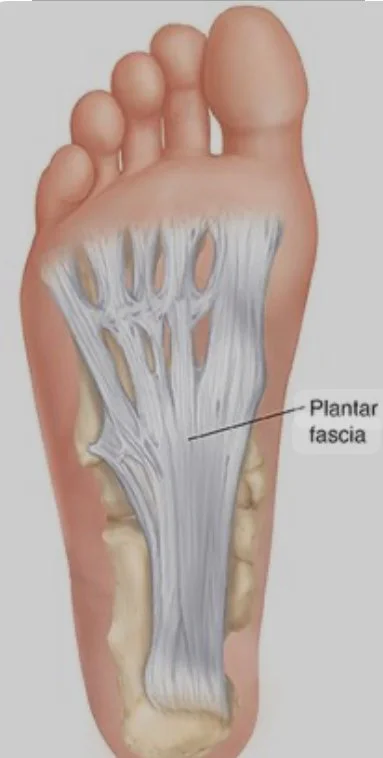
Plantar Fasciitis is one of the most common conditions causing heel and foot pain. The Plantar Fascia is the tough, fibrous tissue running along the sole of the foot, which is attached to the heel bone (calcaneus) and the base of the toes (proximal phalanges). When this vital fascia becomes inflamed or damaged, either from an acute injury, or chronic overuse, it can develop small tears leading to intense pain and discomfort. The most telltale sign of Plantar Fasciitis is sharp, stabbing pain, especially upon the first steps in the morning.
Whom Does Plantar Fasciitis Affect?
Unfortunately, this condition can affect everyone, but it is most commonly found in people between ages 40 - 60, as the fascia can lose elasticity over time.
-
People with a higher BMI, putting more stress on the fascia, potentially leading to inflammation
Individuals whose jobs require long periods of standing: teachers, nurses, factory workers
Athletes or active individuals: runners, dancers, and other high-impact activities, can over stress the fascia especially if the activity is increased too quickly, or they do not have adequate arch support.
People with high or flat arches
Individuals with tight Achilles tendons or calf muscles
Wearing ill fitting or unsupportive footwear
When is Surgery Required?
It is rare to require surgery. Doctors may prescribe surgical intervention if home care has not provided relief in 6-12 months, or if it is affecting the patient’s ability to work or perform moderate exercise. The patient is placed under general anesthesia, and the success rate of the surgeries are 70-90%. The two most common surgeries are:
Gastrocnemius Recession: the surgeon will lengthen the calf muscle to reduce pressure on the plantar fascia
Plantar Fascial Release: the surgeon will make tiny incisions in your plantar fascia to relieve some of the extra tension.
However, there have been reported complications from the surgeries that include collapse of the arch of the foot, nerve damage, lateral column pain, and secondary osteoarthritis in various joints.
Recovery time from surgery can last anywhere from 6 weeks to 6-12 months, depending on the type of surgery and the individual patient.
-
Orthotic arch supports
Splints
Taping the Foot
Icing
Anti inflammatory over the counter medication
Cortisone injections
Shock wave therapy
Radiofrequency ablation, which uses heat to stop the transmission of pain
Acupuncture / Dry Needling
Physical therapy
How can PiIates Help?
Pilates can help with Plantar Fasciitis in two significant ways: It can help you recover from it, but even more importantly, it can prevent it from happening to begin with. Pilates can be preventative in that it strengthens the muscles in the feet, ankles, and lower legs, which are crucial for proper foot alignment; and can reduce strain on the plantar fascia. Additionally, Pilates incorporates targeted stretches that can improve flexibility in the calf muscles, further alleviating plantar fasciitis symptoms.
“Change happens through movement, and movement heals”
Why Pilates Works:
Strengthening the Core: Pilates focuses on developing a strong core, including the deep abdominal muscles, pelvic floor, and lower back. This core strength is integral for maintaining proper posture and weight distribution, thus reducing strain on the feet.
Stretching and Flexibility: Many Pilates exercises promote flexibility in the legs and feet, helping to alleviate tension in the plantar fascia. These gentle, controlled movements enhance the foot’s range of motion and reduce stiffness.
Balanced Muscle Engagement: Pilates is known for its holistic approach to strengthening various muscle groups. This balance ensures that no single muscle or structure is overworked, reducing the risk of overuse injuries.
Key ways Pilates helps with plantar fasciitis:
Muscle Strengthening: Pilates exercises focus on engaging small muscles in the feet and lower leg, improving their stability and function, which can help distribute pressure more evenly across the plantar fascia.
Alignment Correction: Pilates emphasizes proper whole body alignment, which can help correct imbalances that contribute to plantar fasciitis.
Stretching and Flexibility: Pilates incorporates targeted stretches for the calf muscles and plantar fascia, which can help release tension and improve flexibility, reducing pain.
Proprioception Enhancement: Pilates exercises often involve controlled movements that improve proprioception (body awareness), allowing for better foot placement and gait mechanics.
-
Footwork -less spring tension may be required and massaging the fascia into the footbar; wrapping one foot under footbar, other foot over footbar for a deep stretch
Footwork on the Cadillac - client can see their own feet for lower extremity alignment; watch for pronation/ supination of feet, incorrect knee tracking, and poor hip dissociation
Plantar fascia stretching with a foam roller
Calf Stretches - with both knees extended as well as with a gentle flexion (Spine Corrector)
Lunges focusing on pelvic stability
Lat work with springs
Towel Curling with Toes - can add weight for more resistance
Glute Strengthening Exercises
Proprioception Exercises - single leg balances, utilizing a Bosu ball, bird-dog, walking out into a plank
Vestibular Exercises - moving the head while maintaining balance on a single leg
Bridging/ Elephant/ other weight bearing exercises - lift the toes but keeps the balls of the foot down
Rolling out the foot on a ball - only in the direction from ball of foot to heel
Any exercise that stretches the posterior chain e.g, Spine Stretch, Seated Push Through (Cadillac), Hamstring 1 (Chair), Hamstring Stretch (Ladder Barrel)
-
If the client is in the throes of pain, avoid calf strengthening exercises e.g, flex/ point (prancing) on the reformer, heel raises (standing), ankle articulation (chair) - you can build to it when the pain isn’t as acute
If Feet in Straps is painful, try to position the straps in a way that isn’t directly on the affected area, or modify to Thighs in Straps
Avoid high impact exercises - at Club Pilates, this could mean avoiding Cardio Sculpt Classes and Suspend TRX Classes at the beginning of the recovery process
-
Treat the individual condition
Questions to ask ; what other surgeries/ conditions have you had? How did the surgery go - what was the recovery time?
Pushing them (selves) harder vs, easier
Ultimate goal: creating a strength and movement pattern that can adapt to their lifestyle and keep them healthy
“An Ounce of Prevention is worth a pound of cure.”
Consult a medical professional:
If your client has plantar fasciitis, it's crucial for them to consult a Physician or Physical Therapist to get a proper diagnosis. Once a diagnosis is reached, you can work with your client to develop an individualized plan tailored to their specific needs.
Pilates by Nelina
Joseph R. Ford - Physical Therapist at Advocate Condell Hospital